

A cornea transplant, also known as keratoplasty, is a surgical procedure to replace part or all of a damaged cornea with healthy corneal tissue from a donor. The cornea is the clear, dome-shaped surface that covers the front of the eye and plays a crucial role in focusing light onto the retina.
Corneal transplants are typically performed to restore vision in people with damaged or diseased corneas that cannot be treated effectively with medication, glasses, or contact lenses. Conditions that may require a cornea transplant include corneal scarring, keratoconus (a progressive thinning of the cornea), corneal swelling (edema), corneal dystrophies, and corneal infections.
Restore vision.
Reduce pain
Improve the appearance of a damaged or diseased cornea.
Most cornea transplant operations are successful. But cornea transplant carries a small risk of complications, such as rejection of the donor cornea.
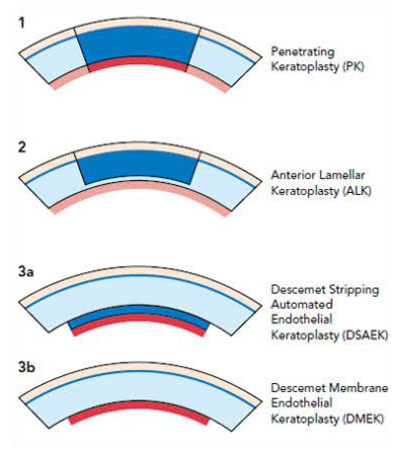
Vision after penetrating keratoplasty (PKP), which is the full-thickness replacement of the cornea, can vary depending on several factors, including the underlying condition being treated, the health of the donor tissue, and the individual healing process.
In the immediate post-operative period, vision is often blurry, and it may take some time for the eye to heal and for vision to improve. Patients typically experience fluctuations in vision during the healing process, with gradual improvement over several months.
Underlying Condition: The reason for the corneal transplant plays a significant role in determining post-operative vision. Conditions like corneal scarring, keratoconus, or corneal dystrophies may have different outcomes.
Type of Transplant: There are different types of corneal transplants, including penetrating keratoplasty (PKP), deep anterior lamellar keratoplasty (DALK), and endothelial keratoplasty (EK). Each type may have different effects on vision.
Healing Process: It takes time for the eye to heal after surgery, and vision may be blurry initially. It can take several weeks to months for vision to stabilize and improve.
Donor Tissue Quality: The quality of the donor corneal tissue can impact visual outcomes. A healthy donor cornea that closely matches the recipient's eye can lead to better vision outcomes.
Complications: Complications such as graft rejection, infection, or astigmatism can affect vision after surgery. Close monitoring and prompt treatment of any complications are essential.
Need for Corrective Lenses: Some patients may still require glasses or contact lenses to achieve optimal vision even after a successful corneal transplant, especially if they had significant refractive errors before surgery.
Corneal transplantation, like any surgical procedure, carries certain risks and potential complications. Some of these risks include:
Graft Rejection: The body's immune system may recognize the donor cornea as foreign tissue and attempt to reject it. This can lead to inflammation, corneal swelling, and vision changes. Graft rejection can often be managed with medications if detected early.
Infection: There is a risk of infection following corneal transplantation, which can lead to significant vision loss if not promptly treated. Patients are typically prescribed antibiotics and instructed to use topical medications to reduce this risk.
Astigmatism: Astigmatism is a refractive error caused by an irregularly shaped cornea. It can occur after corneal transplantation, leading to distorted or blurred vision. Astigmatism may require corrective lenses or additional surgical procedures to address.
Increased Intraocular Pressure (IOP): Some patients may experience elevated intraocular pressure (IOP) following corneal transplantation, which can increase the risk of glaucoma. Monitoring of IOP is important, and medications may be prescribed to manage elevated pressure.
Corneal Graft Failure: In some cases, the transplanted cornea may not integrate properly with the recipient's eye, leading to graft failure. This can occur due to various factors, including infection, trauma, or underlying eye conditions.
Visual Disturbances: Some patients may experience visual disturbances such as glare, halos, or double vision following corneal transplantation, particularly during the initial healing period. These symptoms often improve over time as the eye heals.
Persistent Corneal Disease: SIn some cases, the underlying corneal disease may recur or progress even after transplantation, requiring further treatment or additional surgeries.
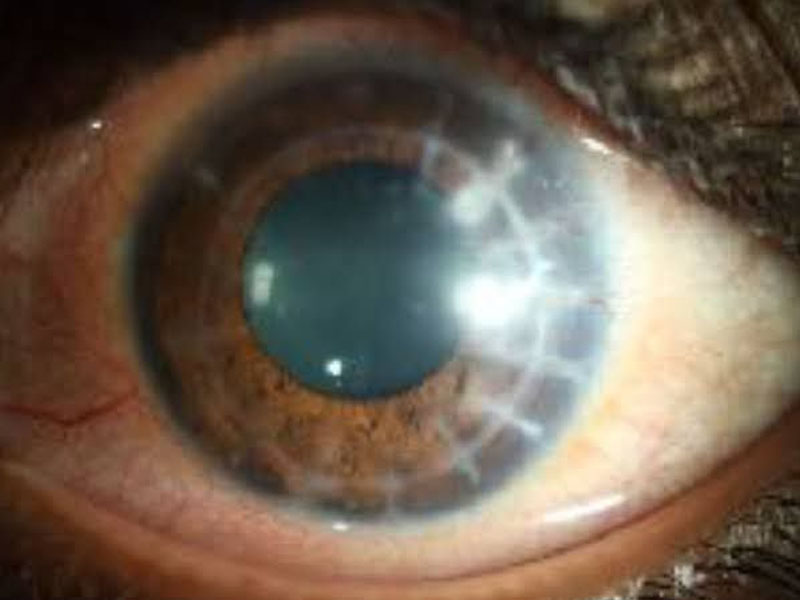
Corneal transplant rejection occurs when the body's immune system identifies the donor cornea as foreign tissue and attempts to attack it. Recognizing the signs and symptoms of corneal rejection is crucial for prompt diagnosis and treatment. Some common signs and symptoms include:
Decreased Vision: A sudden decrease in vision, blurred vision, or distortion may occur if the transplanted cornea becomes swollen or cloudy due to rejection.
Pain or Discomfort: Patients may experience eye pain, discomfort, redness, or sensitivity to light (photophobia) as the immune response causes inflammation in the eye.
Redness: Increased redness of the eye, particularly around the cornea, may indicate inflammation and rejection.
Increased Sensitivity: Sensitivity to light (photophobia) may occur as a result of inflammation in the eye.
Decreased Graft Clarity: The transplanted cornea may become cloudy or hazy, affecting visual clarity.
Tearing: Excessive tearing or watering of the eyes may occur as a response to inflammation.
Foreign Body Sensation:Some patients may feel as though there is something in their eye (foreign body sensation) due to irritation and inflammation.
Corneal Neovascularization: New blood vessel growth (neovascularization) in the cornea may occur as a response to rejection and inflammation.
Graft Edema: Swelling of the corneal graft (graft edema) may occur, leading to decreased vision and discomfort.
If any of these signs or symptoms are present, it is essential for the patient to seek immediate medical attention from their ophthalmologist or eye care provider. Prompt diagnosis and treatment of corneal rejection are crucial for preserving vision and preventing irreversible damage to the transplanted cornea. Treatment typically involves the use of immunosuppressive medications to suppress the immune response and reduce inflammation.