

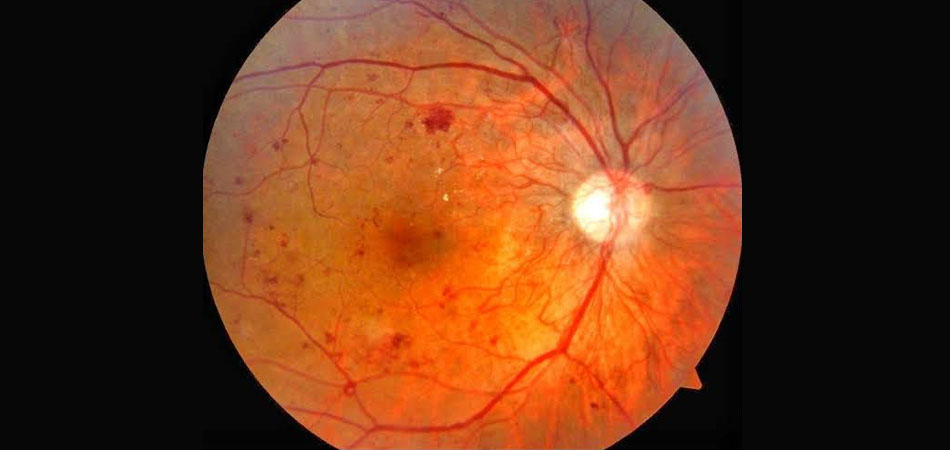
Diabetic retinopathy is a complication of diabetes that affects the blood vessels in the retina, the light-sensitive tissue at the back of the eye. It is a leading cause of blindness among adults with diabetes. Over time, high blood sugar levels can damage the small blood vessels in the retina, leading to various changes that can affect vision.
Non-proliferative diabetic retinopathy (NPDR): In the early stages of diabetic retinopathy, small blood vessels in the retina weaken and develop tiny bulges called microaneurysms. As the condition progresses, blood vessels may become blocked, leak fluid, or bleed into the retina. This can cause blurred or distorted vision.
Proliferative diabetic retinopathy (PDR): In advanced stages, new, abnormal blood vessels may begin to grow on the surface of the retina or optic nerve. These fragile new vessels are prone to bleeding, leading to severe vision loss or blindness if left untreated. Additionally, scar tissue may develop, causing the retina to detach from the back of the eye.
Blurred or fluctuating vision
Floaters (spots or dark strings) in the field of vision
Partial or total loss of vision
Difficulty seeing at night
Colors appearing washed out or faded
Control of blood sugar levels: Keeping blood sugar levels within the target range can slow the progression of diabetic retinopathy and reduce the risk of vision loss.
Laser therapy: Laser treatment can be used to seal leaking blood vessels, reduce swelling, or shrink abnormal blood vessels in the retina.
Intraocular injections: Anti-VEGF medications or steroids may be injected into the eye to reduce swelling and prevent the growth of abnormal blood vessels.
Vitrectomy: In advanced cases with severe bleeding or retinal detachment, surgery called vitrectomy may be necessary to remove blood and scar tissue from the eye.
Early detection and timely intervention are crucial in managing diabetic retinopathy and preventing vision loss. People with diabetes should have regular comprehensive eye exams, at least once a year or as recommended by their eye care provider. Additionally, maintaining good control of blood sugar, blood pressure, and cholesterol levels is essential in reducing the risk and progression of diabetic retinopathy.